Results in 24-48 hours.
Please schedule online and we will determine the best test for you upon arrival.
We perform nasal swabs for COVID, Flu & RSV PCR testing. We also perform antigen testing.
All results PCR and Antigen are available on the same day.
We are testing all those interested in knowing their results
To get tested, please schedule a brief telemedicine visit to determine the best test for you at which time, we will schedule your testing.
Please schedule your visit and we will determine the best test for you upon arrival!
Symptoms of COVID-19 appear anywhere from 2 to 14 days after exposure.
Symptoms that may appear 2-14 days after exposure to the virus:
Cough
Shortness of breath or difficulty breathing
Or at least two of the following:
Fever
Chills
Repeated shaking with chills
Muscle pain Headache
Sore throat
New loss of taste or smell
If you develop any of these emergency warning signs for COVID-19, get emergency medical attention immediately: Trouble breathing
Persistent pain or pressure in the chest
New confusion or inability to arouse
Bluish lips or face
Average incubation 5-6 days (range 1-14)
From onset to max illness – usually about a week.
Recovery is about 2 weeks for mild to moderate disease but 3-6 weeks for severe disease.
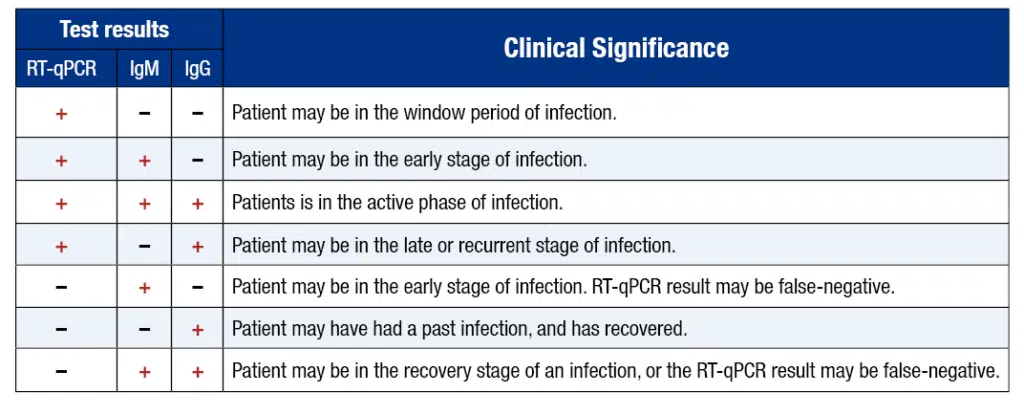
Active COVID-19 infection Day 1-14 after symptom onset -nasal swab RT-PCR testing – allows for early case identification and informing close contacts, reducing spread at home or work
IgM antibody response to COVID-19 Day 7-21
IgG antibody response to COVID-19- after day 14- informs of the presence of an antibody response
Importantly, individuals who had a mild flu like illness that was in fact, COVID-19 -these individuals would have antibodies.
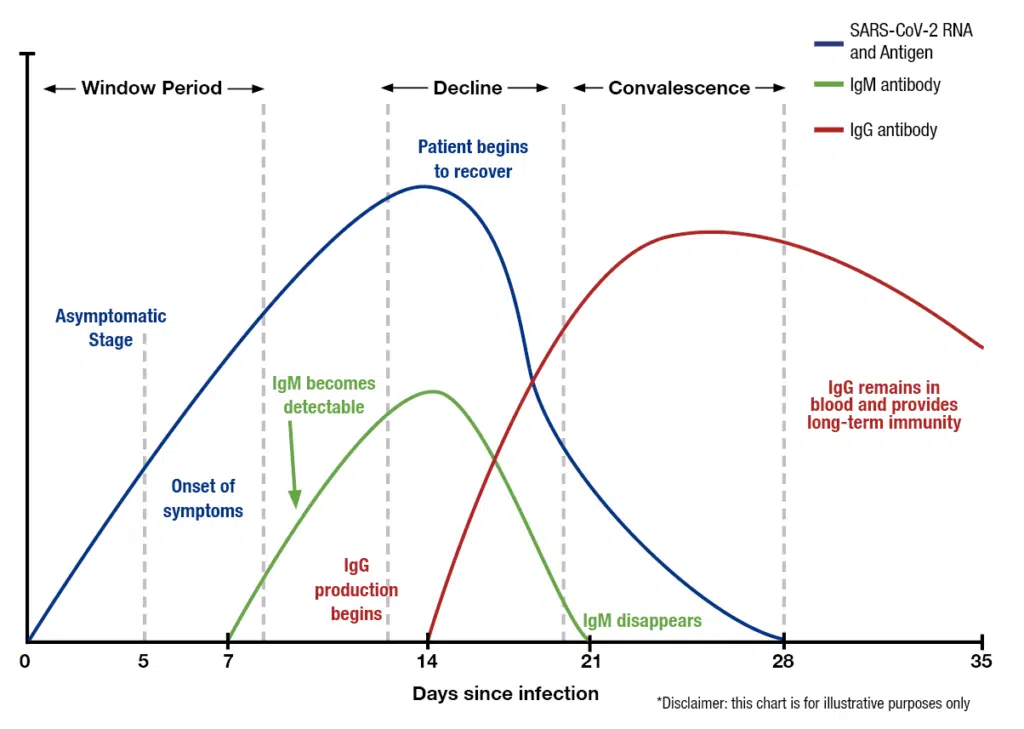
Timing Is Critical For Correct Testing
Day 1-14 since onset of symptoms: Nasal swabs – COVID-19 (RT-qPCR)
Day 14-21 after symptom onset: Nasal swab + IgM antibody blood test for COVID-19
After Day 21 after symptom onset: IgG antibody blood test for COVID-19
Antibody testing should be performed only in individuals after symptom resolution to avoid false-negative results
There are now two ways to test for COVID, Flu or RSV: one that measures the actual virus, and one that measures the body’s reaction to the virus.
The first is a genome test that detects the presence of viral genes in the body using a swabbed sample, usually taken from the nose and throat. The sample is then sent to a lab where it can be replicated and analyzed in a PCR machine. RT-PCR technology plays a role especially in the early stage of a viral infection, in which the virus reproduces quickly. Results take anywhere from one to three days to deliver. Point-of-care genome tests have also been developed that can potentially shorten this waiting period to mere minutes; however, their accuracy at this time is questionable.
The second, which only recently has received FDA approval in the United States, is an antibody test, or serology test, that detects the presence of SARS-CoV-2, Flu A/B or RSV specific antibodies in the blood. Instead of a nasopharyngeal swab, results are obtained using a finger prick blood test. Like the nasal swab test for COVID, Flu & RSV viral genes, the sample is processed in an FDA approved high-throughput lab and results come back in one to three days.
We face a “Tripledemic” this Winter. Your symptoms may be due to the flu, COVID, RSV, or a combination of 2 or 3 of the viruses. All 3 have similar symptoms, hence, it is crucial to know the exact cause of infection.
The flu and COVID can be treated – in fact it is important to treat these early with Tamiflu or Paxlovid to reduce intensity. RSV in this season is affecting adults as well and is a cause of hospital admission. Getting tested is the best approach to determine which infection you have.
COVID-19 PCR TEST
Rapid antigen and RT-PCR tests differ in their analytic sensitivity. Typically, the sensitivity of antigen tests is 30% to 40% lower than for RT-PCR, depending on whether tested subjects were symptomatic or asymptomatic [reference]
However, lower sensitivity has both disadvantages and benefits.
The primary disadvantage is a risk of falsely negative results in people with low viral loads who may be early in their infection, and who go on to spread it to others in subsequent days. In practice, this subpopulation represents just a small fraction of those tested, and risk can be mitigated through serial testing algorithms. There is also a slightly elevated rate of false positives relative to molecular tests, though the rate is dependent on the prevalence of disease and the proportion of people who are symptomatic. A paper published in Lancet, Infectious Diseases noted that for many commonly-used rapid antigen tests, the negative predictive value (e.g., the likelihood someone with a negative test is truly negative for infection) is greater than 98%. [reference]
A major advantage of these assays is the lower likelihood of detecting residual viral nucleic acid left over from a remote infection in recovered individual. This reduces the chance of unnecessary initiation of isolation and quarantine precautions and subsequent rounds of testing.
Rapid antigen tests are subject to the same considerations as the PCR tests with respect to factors that affect clinical sensitivity. These include the quality of sampling and the timing of testing relative to the onset of infection. The CDC advises that rapid antigen tests can have a lower performance in the asymptomatic population, which may be related to the lower levels of virus in this group relative to those with symptoms, rather than characteristics of the tests themselves [reference]
Nucleic Acid Amplification Tests (NAATs) such as RT-PCR for SARS-CoV-2, Influenza A & B or Respiratory Syncytial Virus (RSV) are designed to detect viral RNA. A positive result is highly specific for the presence of COVID-19, Flu or RSV viral nucleic acid. However, it is very important here to note that a positive RT-PCR test does not differentiate between viable and nonviable virus. Thus, a positive test does not necessarily indicate that a person is infectious and requires isolation.
A variety of gene targets are available across different assays, including the envelope gene, the nucleocapsid gene, the ORF1ab gene, and the spike gene. Most assays are designed to detect two or more gene targets. The FDA maintains an up-to-date list of assays with emergency use authorization. [reference]
The RT-PCR’s clinical sensitivity is affected by the assay’s limit of detection, the time since infection began, and sample type. Because patients with symptoms tend to present earlier in their infection course, there is increased test sensitivity in symptomatic people relative to asymptomatic people. Traditionally the nasopharynx has been the preferred body site for sampling, but given patient discomfort and the need for serial testing, many hospitals, and public health programs now use anterior nares or saliva as the primary sampling type.
All symptomatic individuals suspected of having COVID-19, Flu or RSV;
Asymptomatic individuals with known or suspected contact with a COVID-19, Flu or RSV case;
Asymptomatic individuals when the results will impact isolation/quarantine/personal protective equipment usage decisions, dictate eligibility for surgery, or inform the administration of immunosuppressive therapy.
NAAT testing in symptomatic people, even when clinical suspicion is low;
NAAT testing in asymptomatic individuals with known or suspected exposure to COVID-19, Flu & RSV, those requiring hospitalization when community prevalence is high or prior to solid organ or stem cell transplantation and time-sensitive surgeries;
Repeating viral RNA testing when the initial test is negative in symptomatic individuals with intermediate or high clinical suspicion;
Specimen collection from the nasopharynx, mid-turbinate, anterior nares, or combined nasal/oropharyngeal over oropharynx alone.
NAAT testing recommended for older children and adults for RSV due to the lower viral load in their respiratory specimens, making antigen testing less sensitive for this age group.
The COVID-19 & Flu antibody test looks for IgM and IgG antibodies in the blood to determine if your body has already responded to the novel coronavirus or if you have not developed antibodies (you have a higher risk of getting the virus if you do not have antibodies).
Nasal swab: Quest Diagnostics performs the nasal swab RT-PCR. Quest reports that the concentration of SARS-CoV-2 RNA that was successfully detected with at least a 95% detection rate was calculated as 136 copies/mL. It is important to note that timing and adequate sampling determine this test’s sensitivity. Recent data show that RNA positive rates peaked in upper respiratory tract specimens at 7–10 days after symptom onset and then steadily declined after that. Sensitivity also depends on an adequate sample being collected and the disease having advanced enough to have a higher number of viral RNA copies.
IgG antibodies: We offer the Roche Elecsys Anti-SARS-CoV-2 igG Total Antibody test. Roche reports an overall test specificity of 99.81 % (99.65 – 99.91 %) and a sensitivity in patients 14 days after PCR confirmation to be 100% (88.1 – 100 %).
Both, Quest Diagnostics and Roche offer testing in accordance with the FDA Emergency Use Authorization Guidance.
Antibody tests, also known as serology tests, differ from the nasal- and throat-swab tests that can spot a current infection. Instead, these look for signs in the blood that the immune system had fought off an infection in the past.
But there are limits to what antibodies can reveal. With other infectious diseases, antibodies signal a measure of protection against getting sick again. No one knows if that is true of this virus, or, if it is, how long such immunity might last.
A positive test result with the qSARS-CoV-2 IgG/IgM test indicates that antibodies to SARS-CoV-2 were detected, and the patient has potentially been exposed to COVID-19. When IgM antibodies are present, they can indicate that a patient has an active or recent infection with SARS-CoV-2. IgG antibodies develop later following infection, and generally do not begin to appear until 14-21 days after infection. When IgG antibodies are present it, often indicates a past infection but does not exclude recently infected patients who are still contagious, especially if detected with IgM antibodies.
Since most patients do not know the exact time when they contracted the virus, the combining both IgM and IgG tests provides a much higher test sensitivity and test specificity.
The presence of antibodies and immunity
It is unknown how long IgM or IgG antibodies to SARS-CoV-2 will remain present in the body after infection and if they confer immunity to infection.
If you think you might have been exposed to the COVID-19, please schedule your appointment immediately.
COVID-19, Flu & RSV Nasal Swab RT-PCR Test: The sensitivity of this test is low in early illness, and is even lower in asymptomatic individuals, likely because of lower viral load, which means even more false negatives. The test’s sensitivity is also dependent upon obtaining an adequate sample from inside the nose. Sensitivity of RT-PCR is likely to be higher later in the illness when the viral load is higher.
COVID-19 & Flu Antibody Tests: Antibodies may not be present in detectable levels in early days of an infection. Test sensitivity increases with the time from from onset of symptoms and is more sensitive later. Delaying a test for too long may not be fruitful because at this time, we do not know how long IgM or IgG antibodies to SARS-CoV-2 or Influenza A & B will remain present in the body after the infection has been cleared.
One potential use of COVID antibody tests is to measure the extent of the pandemic at the population level. Our understanding of the disease and its projected impact in the US is weakened by our inability to monitor its spread among people with either mild symptoms or none at all.
Another use is to measure the progress of individual infection. Antibody tests quantify the number of immunoglobulin M (IgM) and immunoglobulin G (IgG) antibodies in the blood. The presence of more IgM antibodies, which are the first to appear and mobilize against an invading organism, indicates more recent exposure to the virus. It is through this result that an asymptomatic carrier of the virus could be identified—a feature of no small importance, since “silent carriers” have played a major role in transmission.
More IgG antibodies, which are virus specific and produced in later stages of infection, would lead a person to test positive for immunity, implying recovery. This unfortunately doesn’t guarantee full protection. The test won’t reveal how neutralizing, or how potent, these IgG antibodies are; nor can it determine how long they will last. With certain families of coronaviruses, including the beta coronavirus family that includes SARS-CoV-2, reinfection has been found to occur, and for now it remains a possibility.
Successful deployment of antibody tests depends on their “sensitivity and specificity.” Sensitivity prevents false negatives, since a more sensitive test is more likely to actually detect it. Specificity, on the other hand, prevents false positives, since a less specific test may pick up on antibodies against a virus other than SARs-CoV-2.
It would take a concerted effort, but in the United States we have the infrastructure and manpower it takes to conduct rapid antibody tests quickly, cheaply, and at a massive scale. The small European country of Andorra has plans to give antibody tests to its entire population. Compared to other resource rich nations, we’ve failed to answer the WHO director general’s call to “test, test, test.” That can change—but only if we act now, and act fast.
IF YOU RECEIVED
Pfizer-BioNTech or Moderna
Who should get a booster:
Everyone 18 years or older
When to get a booster:
At least 6 months after completing your primary COVID-19 vaccination series.
Which booster should you get?
Any of the COVID-19 vaccines authorized in the United States.
——————————
IF YOU RECEIVED
Johnson & Johnson’s Janssen
Who should get a booster:
Everyone 18 years or older
When to get a booster:
At least 2 months after completing your primary COVID-19 vaccination.
Which booster should you get?
Any of the COVID-19 vaccines authorized in the United States.
VACCINATION LOCATION: 3264 N Lincoln Ave, Chicago, IL 60657
Yes. Everyone is still considered fully vaccinated two weeks after their second dose in a two-shot series, such as the Pfizer-BioNTech or Moderna vaccines, or two weeks after a single-dose vaccine, such as the J&J/Janssen vaccine.
Bring your CDC COVID-19 Vaccination Record card to your booster shot appointment so your provider can fill in the information about your booster dose. If you did not receive a card at your first appointment, contact the vaccination site where you got your first shot or your state health department to find out how you can get a card.
You may experience side effects after getting a COVID-19 vaccine. These are normal signs that your body is building protection against COVID-19.
Use v-safe to tell CDC about any side effects. If you enter your booster shot in your v-safe account, the system will send you daily health check-ins.
Vaccines available: Moderna & Pfizer
Although COVID-19 vaccination remains effective in preventing severe disease, recent data suggest vaccination becomes less effective over time, especially in people aged 65 and older and at preventing infection or milder illness with symptoms.
The recent emergence of the Omicron variant (B.1.1.529) further emphasizes the importance of vaccination, boosters, and prevention efforts needed to protect against COVID-19. Early data from South Africa suggest increased transmissibility of the Omicron variant and the potential for immune evasion.
Emerging evidence also shows that among healthcare and other frontline workers, vaccine effectiveness against COVID-19 infections is also decreasing over time.
This lower effectiveness is likely due to the combination of decreasing protection as time passes since getting vaccinated, as well as the greater infectiousness of the Delta variant.
Data from clinical trials showed that a booster shot increased the immune response in trial participants who finished a Pfizer-BioNTech or Moderna primary series 6 months earlier or who received a J&J/Janssen single-dose vaccine 2 months earlier. With an increased immune response, people should have improved protection against COVID-19, including the Delta variant. For Pfizer-BioNTech and J&J/Janssen, clinical trials also showed that a booster shot helped prevent COVID-19 with symptoms.
Coadministration with Other Vaccines:
COVID-19 vaccine booster dose (Pfizer-BioNTech, Moderna, or Janssen) may be given with other vaccines, without regard to timing.
▪ This includes simultaneous administration of COVID-19 vaccines and other vaccines on the same day.
▪ If multiple vaccines are administered at a single visit, administer each injection in a different injection site.
Not at this time. We only offer Moderna & Pfizer.
So far, reactions reported after getting a booster shot were similar to those of the two-shot or single-dose primary series. You can use v-safe to tell CDC about any side effects. If you enter your booster shot in your v-safe account, the system will send you daily health check-ins. Fever, headache, fatigue and pain at the injection site were the most commonly reported side effects, and overall, most side effects were mild to moderate. However, as with the two-shot or single-dose primary series, serious side effects are rare, but may occur.
Lakeview
3264 N Lincoln Ave
Chicago, IL 60657
(424) 282-6843
Wicker Park
1601 W Division
Chicago, IL 60622
(424) 282-6843
Open 7 Days
Mon-Thu: 8a-7p
Fri-Sat: 8a-5p
Sun: 9a-5p
Lakeview
3264 N Lincoln Ave
Chicago, IL 60657
(424) 282-6843
Wicker Park
1601 W Division
Chicago, IL 60622
(424) 282-6843
Open 7 Days
Mon-Thu: 8a-7p
Fri-Sat: 8a-5p
Sun: 9a-5p
This website uses cookies to ensure you get the best experience. See our Privacy Policy to learn more.