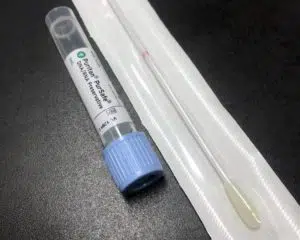
Point of care testing during infectious outbreaks, especially the COVID-19 pandemic, has become a first line modality for rapid detection and prevention. Testing after exposure, new-onset symptoms, or being unmasked in a crowded space is especially important as COVID-19 is highly transmissible. Even for individuals that are asymptomatic, unvaccinated, or without any symptoms but have had exposure, testing is recommended. Currently, the point of care test that is used most often in the detection of the virus is called the Rapid Antigen test.
Many people have had a rapid antigen test over the last two years during the COVID-19 pandemic. This test is performed via bilateral swabs of the nasal mucosa and tissue to assess for the presence of the COVID-19 antigen. A positive antigen result indicates infection. This test is the fastest test we have to date, with a turn-around time of two hours. It is useful in early detection for the prevention and treatment of an outbreak.
With increased utilization and importance of early testing, the rapid antigen has become pivotal in the current pandemic. Thus, it is important to ensure that this modality is accurate and yields correct results. Furthermore, it is necessary to understand whether the rapid antigen is a sensitive or specific test. By definition, a specific test is one that is better able to differentiate an illness, or “rule it in,” and a sensitive test is a test that can easily pick up the presence of an illness, so it is good at “ruling it out.” By understanding the characteristics of a test and how accurate it is, providers and patients are more likely to have better outcomes and treatment plans.
A recent Cochrane review of studies titled, “Rapid, point‐of‐care antigen and molecular‐based tests for diagnosis of SARS‐CoV‐2 infection,” evaluated the accuracy of the rapid antigen test in symptomatic vs. asymptomatic individuals. The results concluded that the rapid antigen test is more accurate in diagnosing COVID-19 in individuals with symptoms than without. Specifically, in confirmed COVID-19 cases, the “antigen test(s) correctly identified COVID‐19 infection in an average of 72% of people with symptoms, compared to 58% of people without symptoms.” The timeline of infection was found to be an important factor in accuracy as well. Researchers reported an increase in accuracy of the test when it is conducted in the first week after symptom development despite the presence of symptoms. Specifically, the rapid antigen test “correctly ruled out infection in 99.5% of people with symptoms and 98.9% of people without symptoms.”
However, the rapid antigen is not as good as the RT-PCR test, or the molecular test. Research shows that because the sensitivity of an antigen test so heavily relies on timing, the likelihood of a false negative is 20% higher than the RT-PCR. Thus, where there is high clinical suspicion for active COVID-19 infection, a negative rapid antigen test should be followed with a RT-PCR test. Similarly, a rapid test can be used in combo with a PCR if there is high concern for isolation and contact tracing.
So, how do we define how good a rapid antigen test really is? The answer is mixed. A rapid antigen test is a good test if certain criteria is met, but when compared to the RT-PCR test, it is not as good. Specifically, research found that the RT-PCR identified 95.1% of infections correctly and 99% were correctly ruled out, regardless of the presence of symptoms. In comparison, rapid antigen tests had a 72% and 58% accuracy rate respectively, and this depended on symptom presence. Thus, the RT-PCR is more specific and sensitive, whereas the rapid antigen is only substantially sensitive within 7 days of exposure or symptom onset and is dependent on more criteria.
In conclusion, a COVID-19 rapid antigen test is a good test during the first seven days after exposure or symptom onset. It is also a preferred test over the RT-PCR when time is the priority, as it is more accessible and provides results more quickly. Furthermore, its sensitivity during the crucial seven day time period may “increase detection and speed up isolation and contact-tracing, leading to reduction in disease spread and reduce the burden of laboratory services” (Cochrane, et al). Although it is not as accurate as the RT-PCR, and is dependent on more factors, the rapid test is a good point of care test, and it has improved the outcomes and reduced transmission rates during the COVID-19 pandemic.
Link: